Grace Wright. MD, PhD Reviews Challenging Cases of Rheumatic Diseases - Episode 3
Case Study 3: Non-Radiographic Axial Spondylia Patient Case Overview and Therapeutic Goals
Transcript:
Wright, MD: This is our third and final case. Hopefully, we can have a more robust discussion with this one, as well. We have a 21-year-old woman who comes to our primary care provider with severe lower back pain that wakes her up in the middle of the night, and she has attributed the pain herself to her active athleticism and mentioned that the pain subsides when she starts moving around. On exam, she’s got some tenderness in the lumbar spine, decreased range of motion and lumbar spine, and her provider seems to think that she’s got lumbar strain and does the same thing as the other guy did. He starts ibuprofen 400 mg 3 times daily with physical therapy.
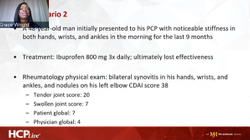
Four weeks later, she still has her back pain. She gets a little bit of relief, but it doesn’t last long. She is still waking up. Her mobility, and productivity are again diminished because of her back pain. She has developed some diarrhea, some vomiting, and some abdominal pain. Now folks are worried, imaging is done, and she gets an x-ray done of her spine that shows a mild degenerative disc disease from her years, at this point it’s 10 plus years, of various forms of athletics. On exam her c-reactive proteins are 4.7. Sedimentation rate is 38, and she is B27 positive.
The truth is that we don’t have a good way to prognosticate these patients; 8% will not go on to ankylosis, except for those who have syndesmophytes. Even if they are asymptomatic, if they have syndesmophytes, then the likelihood of having more aggressive structural damage is enhanced.
On the left we have her normal x-ray with no erosions on anchylosis, and on the right, she has bone marrow edema. She brought up a very good point that she’s an athlete, and athletes can develop an MRI that looks just like that, so we now have that conundrum. Is this her mechanical activity, or is this purely inflammatory? I don’t know if there’s any way at this particular point in time to separate those 2.
I just brought in the 3 that we now have approved for radiographic, and I think we’re all agreed that this is nonradiographic. I don’t think there’s any debate on that, so we have the CX SPAN, prevent, and the COAST X. Two things that I find interesting are the trial designs here. Number 1 is the primary endpoint as is your 52 weeks. That’s what the agency has required. Number 2, there are no prespecified movement for the placebo arm, so as you see patients moving up into whatever the active comparator is throughout the course of the time so when you look at the final output for me sometimes it can be a bit of a mishmash because of where the patients travel.
When they do the data analysis, where they look at the individual patients and how they’ve traveled through you will see the settling of the disease activity burden within the cohorts. That sometimes for me can be more impactful than looking at a bar graph just because of the difference in the way these trials are designed compared to all the others.
That being said we’ve got certolizumab on the top left, PREVENT on the top right, and COAST-X on the bottom. We’ll see CX SPAN which is the first to get the approval for certolizumab: 57% versus 16% at 52 weeks. PREVENT trial results just came out, and it is looking at 2 different ways of administering. We have secukinumab with load secukinumab without load. There are very little difference with the numbers, and the placebo arm compares quite similarly. Then when we look at COAST-X with ixekizumab 80 mg compared to placebo 31% and 13%.
At least we know we now have data that says this is effective. There is an ICD-10 code that is for this treatment. We’ve got data and the safety profiles. I’m not going to belabor this because we looked at this before. There are no difference from the current standings, so we’ve got data, so there’s really nothing that says we need to waddle around in oral, conventional, synthetic disease-modifying anti-rheumatic drug world for an axial predominant disease even if they have proliferative arthritis.
Transcript Edited for Clarity